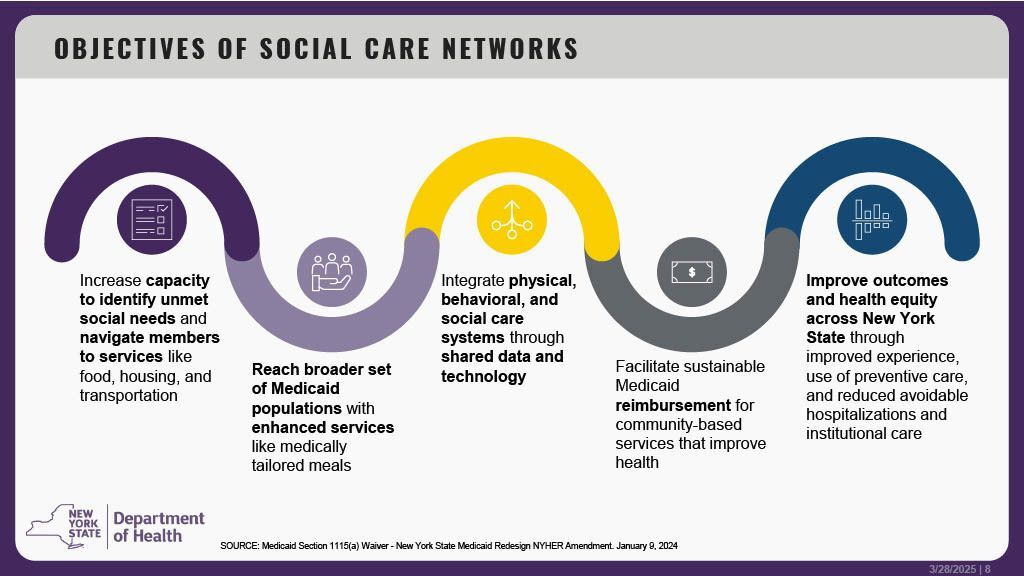
Social Care Networks (SCN)
You may be eligible for free help with food, housing support, or transportation!
MHAOC is a proud partner of the Hudson Valley Social Care Network https://hvcare.org/scn. This new program addresses health disparities in low-income communities by leveraging federal funding to facilitate Medicaid members’ access to nutritional meals, housing supports, transportation and other social services that can have a significant impact on an individual’s health.
If you or a family member is enrolled in Medicaid, you may qualify for additional services through Hudson Valley’s Social Care Network – Even if you’re already enrolled in a Health Home.
Get started today! Find out what you’re eligible for—it’s simple and confidential.
Call 845-342-2400 or email ccoordination@mhaorangeny.com.
Complete a short screening and eligibility form.
Get connected to services! Or, complete an online self-screening form at https://hvcare.org/scn .
Talk to us or your care manager about taking a brief confidential screening to see if you’re eligible to receive new and expanded free services, including:
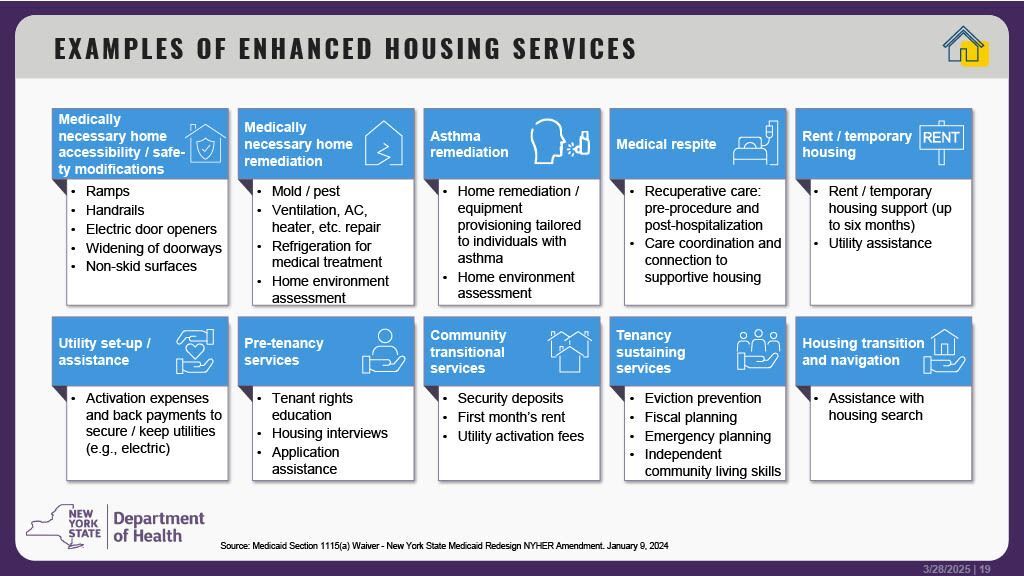
Housing Support
- Help with rent and utility payments
- Housing search
- In-home health and safety support
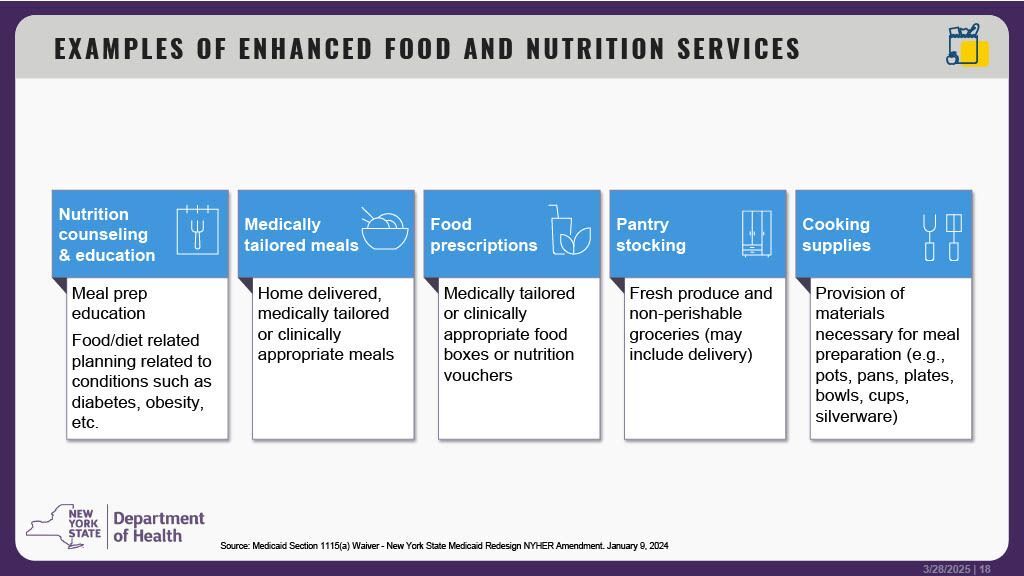
Food Assistance
- Healthy meals
- Cooking supplies
- Nutrition planning
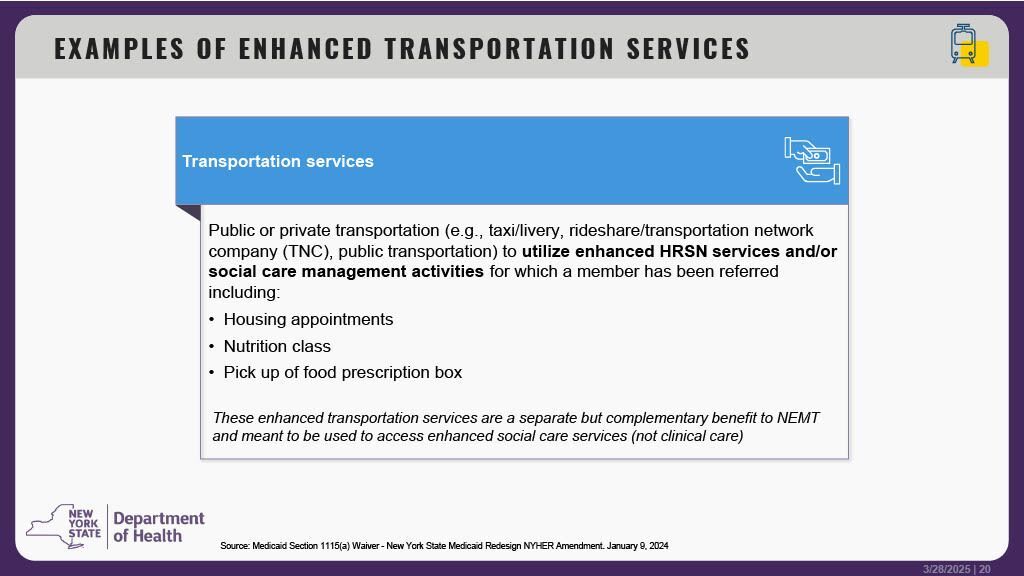
Transportation Help
- Rides to non-medical appointments like job interviews, housing appointments, government offices, and more.
- Support with public or private transit options
Referral Form: https://mhaorangeny.forms-db.com/view.php?id=123395